Over the next 25 years, Canada’s baby boomer population will continue to reach age 65 and older and, here in B.C. – according to Statistics Canada – the senior population is set to exceed the national average.
“The silver tsunami is a real epidemiological phenomenon that we are only experiencing the first ripples of,” says David Sherman, a UBC medical resident and one of only four physicians in its geriatric psychiatry program. “Our society is going to have the kind of aging population that we’ve never seen before.”
With this surge of aging ‘boomers,’ B.C.’s doctors will begin to see an increased number of ‘complex cases’ – individuals faced with a myriad of medical, mobility, and psychological issues, ranging from dementia and depression through to anxiety.
But here at UBC’s Faculty of Medicine, subspecialty residency training programs like geriatric medicine and geriatric psychiatry, have heard the alarms and are equipping the next generation of doctors with the skills and expertise to support the wave of aging baby boomers.
Geriatric medicine residents learn to ‘pull together all the piece
Among this next generation of doctors is Martha Spencer, a fifth-year resident completing her final year of training in geriatric medicine.
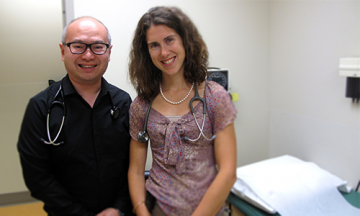
L-R: Roger Wong, Associate Dean of Postgraduate Medical Education, and geriatric medicine resident Martha Spencer.
“I grew up as an only child and developed a very close relationship with my grandparents,” says Dr. Spencer, recalling summers spent on the open road with her parents and grandparents. “From an early age, I learned to relate to older people and that’s where my love of helping elderly people and geriatrics began.”
Originally from Corner Brook, Newfoundland, Dr. Spencer says it was the focus on acute geriatric medicine that attracted her to UBC’s geriatric medicine subspecialty residency training program.
Over the course of the two-year program, geriatric medicine residents, like Dr. Spencer, are exposed to a wide range of rotations in everything from in-hospital acute consultation, rehabilitation, community, and long-term care geriatrics.
Residents also gain experience conducting outreach in rural, remote and northern communities – including Haida Gwaii, Prince Rupert, and Prince George. Lawrence Lo, Program Director of the geriatric medicine training program, says he sees these outreach experiences as vital to residents’ overall development.
“It’s an eye-opening experience,” says Dr. Lo. “These outreach opportunities bring residents face-to-face with individuals who are in need of services and the hope is that it will impact how they advocate for patient populations going forward in their career.”
Dr. Spencer just recently returned from a trip to Haida Gwaii, where she worked with a local family doctor to conduct consultations with older patients in the community.
“Geriatricians work collaboratively with family doctors and can really help provide support with their more complex patients,” Dr. Spencer says.. “In geriatrics, there are so many aspects of the patient that we look at – not just the medical piece, but the functional piece, the mobility piece, and the cognitive piece. Having someone to pull together all the pieces is important, and that’s the role of the geriatrician.”
But in order to ‘pull together all the pieces’ and approach healthcare from a holistic vantage point, geriatricians need to be working with teams of generalists, specialists and allied health professionals.
Working as a team
For Dr. Spencer, it was this ‘team-based’ approach that drew her to the profession in the first place.
“I love working in a team – that’s one of things that I love so much about geriatrics,” Dr. Spencer says. “Because older patients can be very complex, you really can’t do it alone.”

Geriatric psychiatry resident David Sherman
This sentiment is echoed by her colleagues in the geriatric psychiatry subspecialty training program, which gives residents the tools and expertise to assess, diagnose and treat older patients with complex mental disorders.
“Geriatric psychiatry requires a multi-disciplinary team approach,” says David Sherman, whose interest for the subspecialty “blossomed” during a core rotation during year three of his postgraduate training. “I had a wonderful experience working with all the members of the geriatric team – not just the psychiatrists, but the family physicians, nurses, physiotherapists, occupational therapists and pharmacists.”
Jeanine Marshall. a graduate of the Island Medical Program now completing UBC’s geriatric psychiatry training in Victoria agrees: “At the end of the day, elderly patients have such complex issues and it’s difficult for anyone to work in isolation – multidisciplinary teams are needed to serve the aging population.”
Providing specialized support
According to Martha Donnelly, Director of the geriatric psychiatry residency training program, when it comes to caring for older patients with complex mental health needs, geriatric psychiatrists are vital to the team.
“We not only have a tsunami of older patients, we have tsunami of dementia,” says Dr. Donnelly, who built UBC’s geriatric psychiatry program from the ground up and witnessed its official launch in 2012.
“Geriatric psychiatrists have the expertise – but also the time to handle some of these complicated problems,” she says. “We have shorter waitlists than general psychiatrists and can prioritize to see patients within a few days – or the same day – if necessary.”
The important role that specialist and subspecialists play in the overall healthcare system is widely recognized.
“A sustainable healthcare system includes the training of specialty and subspecialty physicians,” says Roger Wong, Associate Dean of Postgraduate Medical Education. “The growth and demographics of B.C.’s population means that demand for physicians trained in subspecialties, particularly those who focus on medical conditions affecting the aging population, will continue to increase.”
Training the next generation
For Dr. Donnelly, readying the next generation of geriatric psychiatrists is what keeps her going.
“It’s very gratifying to be teaching the next generation,” Dr. Donnelly says.
And it’s not just about teaching residents to diagnose and treat the ‘textbook cases’ – it’s about teaching them to truly know the people they’re caring for.
“I’ve often said to medical students: when I see a patient and take a history – it’s like reading a biography. These people have had very interesting lives – often 85, 90…sometimes 100 years of it. It’s extremely exciting to know about some else’s life and see that you can make a difference.”

L-R: Geriatric psychiatry residents Jeanine Marshall, Nadeesha Fernando, Paul Blackburn and David Sherman with Program Director Martha Donnelly at September’s Canadian Academy of Geriatric Psychiatry and Canadian Coalition for Seniors’ Mental Health Joint Conference in Toronto.
Dr. Donnelly’s wisdom is beginning to rub off on her residents – although many who enter this subspecialty program appear almost predisposed with a special insight.
“Geriatric patients really offer a rich tapestry of experience and personal history that I have always enjoyed being a part of,” says fifth-year geriatric psychiatry resident Paul Blackburn, who is completing his training in Vancouver.
“This subspecialty really allows me to advocate for older patients,” he says. “Elders are faced with enormous changes in their lives – they may be dealing with bereavement of spouses, retirement after decades of work, dementia, their own mortality – this is incredibly difficult for patients and families to face. And without a little bit of extra training and understanding of how everything fits together, these can be difficult issues for doctors to face.”
UBC residents have received training in geriatric psychiatry through elective and fellowship opportunities since 1984. In 2012, when geriatric psychiatry was formally recognized as a subspecialty by the Royal College of Physicians and Surgeons of Canada, UBC seized the opportunity to meet the province’s health needs, becomeing one of only a handful of medical schools across the nation to offer an accredited geriatric psychiatry subspecialty residency training program.
In addition to clinical training, UBC conducts a wide range of research on diseases associated with the aging demographic. When it comes to Alzheimer’s disease – the most common cause of dementia among older people – a recent donation by Canadian diamond pioneer, Charles Fipke is helping to put UBC at the global forefront of research.
UBC postgraduate subspecialty residency programs
UBC Faculty of Medicine’s postgraduate subspecialty residency programs cover a variety of fields, ranging from gynecologic oncology to critical care medicine. Together, these programs are training physicians who provide specialized skills and knowledge that benefit patients, often with significant health challenges, across British Columbia. Subspecialty-trained physicians also offer support to family physicians providing front-line patient care across the province through professional consultations and referrals. Find out more here.