Scientists in the UBC Faculty of Medicine and Janssen Research & Development LLC have shown for the first time that Type 2 diabetes can be effectively treated with a combination of specially-cultured stem cells and conventional diabetes drugs.
Stem cells – generic cells that haven’t yet taken on specialized form and function – have recently been used by scientists at UBC and elsewhere to reverse Type 1 diabetes in mice. In Type 1, which usually begins in childhood, the pancreas produces little or no insulin, the hormone that enables cells to metabolize sugar (glucose).
These new results, published today in Stem Cell Reports, hold much broader potential because Type 2 diabetes accounts for more than 90 per cent of diabetes cases. In Type 2, which usually arises in adulthood and often stems from poor diet, lack of exercise and obesity, the body’s cells lose their ability to respond to insulin; as a result, glucose accumulates to toxic levels in the blood.
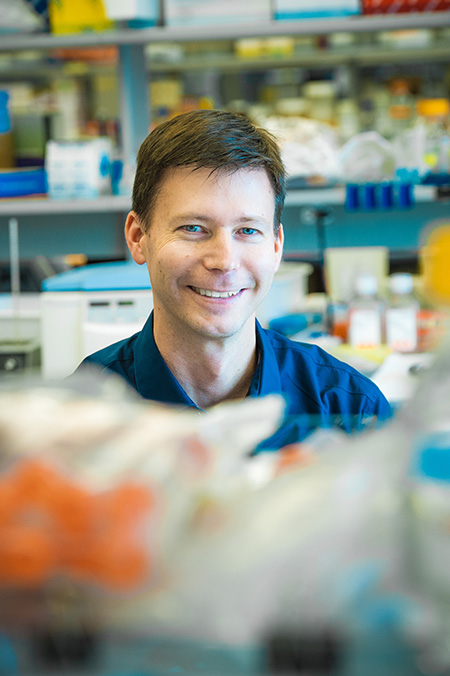
Timothy Kieffer, a professor in the department of cellular and physiological sciences, and scientists from Janssen’s BetaLogics Venture simulated Type 2 diabetes in mice by putting them on a high-fat, high-calorie diet for several weeks. Dr. Kieffer’s team then surgically implanted pancreatic-like cells that had been grown in the laboratory from human stem cells.
Mice that received a combination of the cells with one of three diabetes drugs became as “glucose tolerant” as the healthy mice, meaning they were able to keep their blood sugar in check, even after ingesting a sugary meal. In contrast, a group of mice with simulated Type 2 diabetes that received the drugs but not the transplants remained glucose-intolerant.
“Being able to reduce spikes in blood sugar levels is important, because evidence suggests it’s those spikes that do a lot of the damage – increasing risks for blindness, heart attack, and kidney failure,” says Dr. Kieffer, a member of UBC’s Life Sciences Institute.
The combination therapy also produced an unexpected, but welcome result: the mice returned to a normal weight, the same weight as a healthy control group that had been reared on a low-fat diet.
“Their weight loss was intriguing, because some of the common diabetes therapies often lead to weight gain,” Dr. Kieffer said. “We need to do more studies to understand how the cell transplants lead to weight loss.”
The team is also investigating if higher doses of the cells – beyond the 5 million tested in this study – can achieve the same results without the need for additional drugs.
Almost 400 million people diabetes, and it’s the eighth leading cause of death. It is more common in developed countries and has exploded in frequency during the past few decades, due mostly to decreased activity levels and worsening diets. From 1999 to 2009, the prevalence of diagnosed diabetes among Canadians increased by 70 per cent.
The cheapest, simplest way to treat Type 2 diabetes is through diet and exercise, but this alone is not always effective. Several orally-administered drugs enhance insulin production or improve the body’s sensitivity to insulin, but can lose their effectiveness over time and carry various side-effects. Many patients are put on a regimen of self-injected insulin, but dosing can be difficult to calibrate, and it can promote weight gain.
U.S. and Canadian regulators have approved clinical trials of stem cell treatments for Type 1 diabetes; the first patient received a transplant in October. Perhaps the biggest hurdle will be preventing a person’s immune system from rejecting the transplanted stem cells.
This work was funded in part by the Canadian Institutes of Health Research (CIHR) Regenerative Medicine and Nanomedicine Initiative, the Stem Cell Network (SCN), the JDRF, and Stem Cell Technologies.