Stronger drunk driving law leads to safer roads
Stronger drunk driving law leads to safer roads
Do harsher penalties for drunk driving reduce fatal crashes, hospital admissions and ambulance calls? For Jeff Brubacher, an emergency physician at Vancouver General Hospital, the question is hardly academic.
So he and his colleagues do what academics do – they crunched the numbers.
In a study published in the American Journal of Public Health, Dr. Brubacher, the lead author and an Associate Professor of Emergency Medicine, reported that British Columbia’s ratcheting up of penalties led to a 21 per cent decline in fatal crashes, an 8 per cent decline in crash-related hospital admissions, and a 7.2 per cent decline in crash-related ambulance calls.
Based on those statistics, there were an estimated 84 fewer fatal crashes, 308 fewer hospital admissions and 2,553 fewer ambulance calls for road trauma each year.
The beneficial effects of the new laws were due mostly to a reduction in crashes related to drinking and driving.
Under the changes that B.C. imposed in 2010, drivers who get caught for the first time with a blood alcohol content (BAC) of .05% to .08% have their driver’s license immediately suspended for three days and, at police discretion, may also have their vehicle impounded for three days (instead of the previous one-day suspension and no vehicle impoundment). They also must pay fees of approximately $600, compared to no fine before. Drivers with a BAC higher than .08% have their licenses immediately suspended for 90 days and their vehicle impounded for 30 days.
In the months after the heavier penalties took effect, many owners of drinking establishments complained that the penalties for a BAC higher than .05% were hurting their business. The B.C. Civil Liberties Association (BCCLA) also challenged the new rules in court, arguing that the harsher penalties essentially criminalize drivers who fail a roadside blood-alcohol test or refuse to be tested.
Drawing on previous research, Dr. Brubacher and colleagues assert that the changes to the law and accompanying enforcement and media coverage – and not other factors – were responsible for the reduced rate of fatal crashes, hospital admissions and ambulance calls.
“Our findings add to the growing evidence that the new laws, although controversial to some, were associated with marked improvements in road safety,” says Dr. Brubacher, who is also a Scientist at the Centre for Clinical Epidemiology and Evaluation of the Vancouver Coastal Health Research Institute, and Director of Vancouver General Hospital’s Emergency Medicine Research Division. “We hope that other jurisdictions will follow B.C.’s lead in implementing similar laws designed to deter dangerous driving.”
A broken barrier theory of ALS
The firing of a motor neuron depends on its ability to compartmentalize itself. Christopher Loewen, an Associate Professor in the Department of Cellular and Physiological Sciences, discovered one biochemical recipe for such internal barriers – and in the process, may have revealed a cause of amyotrophic lateral sclerosis (ALS).
Also known as Lou Gehrig’s disease, ALS causes people to lose control of their muscles. In most cases, they die three to five years after symptoms first appear.
But Dr. Loewen’s findings, published in the journal Cell, weren’t based on neurons. Instead, he was using a much simpler organism: yeast.
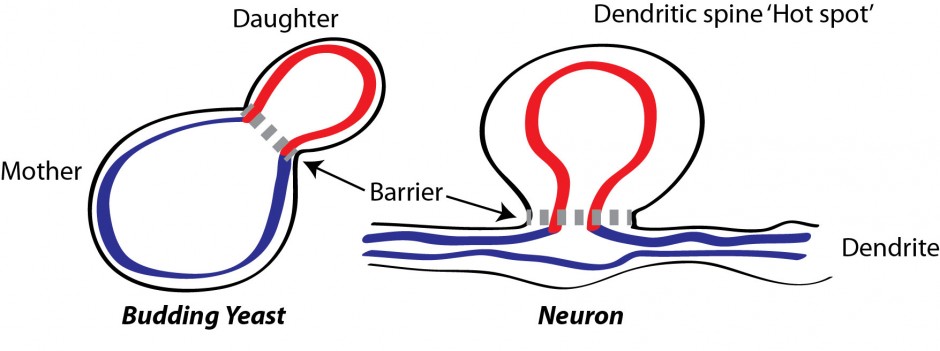
A yeast cell reproduces by squeezing off some of its own material to create an exact copy of itself. To prevent the unwanted mixing of material between “mother” and “daughter” during division, the mother erects a barrier between itself and its daughter. Dr. Loewen found that this barrier is formed by certain proteins in the outer membrane linking up with proteins in the inner membrane (the endoplasmic reticulum).
The same principle applies to neurons. The branches of neurons, known as dendrites, are primed to receive signals from neurotransmitters; effective nerve transmission depends on concentrating the neurotransmitters, such as glutamate, on the spines that protrude from dendrites.
“If you don’t restrict the biochemistry to these hot spots on the spines, it will break down in the tangles of dendrites,” says Dr. Loewen, a member of UBC’s Life Sciences Institute and the Djavad Mowafaghian Centre for Brain Health. “It would be so diluted that it wouldn’t be able fire the neuron.”
One of the dozen mutations that lead to ALS affects production of a protein called VAP-B, which is very similar to one of the linking proteins in yeast identified by Dr. Loewen. He speculates that VAP-B may be a crucial part of the internal barrier isolating the hot spot from the rest of the dendrite. Without VAP-B, the barrier between the hot spot and the rest of the dendrite becomes porous, the glutamate signal leaks out, and the neuron won’t fire.
The next step for Dr. Loewen is to test that theory in animal models with the VAP-B mutation. He and Associate Professor Shernaz Bamji will examine the hot spots of the specimens’ dendrites to see if signaling at those points is degraded.
The dark side of antibiotics
Many antibiotics, for all their therapeutic power, don’t discriminate – they attack all kinds of microbes, even the ones we need. So understanding how different antibiotics affect those helpful bacteria is just as important as understanding how they kill the harmful ones.
Kelly McNagny, a Professor in the Department of Medical Genetics, has found that receiving antibiotic treatments early in life can increase susceptibility to specific diseases later on.
In the study, published in the Journal of Allergy and Clinical Immunology, he and Brett Finlay, a Professor in the Department of Biochemistry and Molecular Biology, tested the impact of two antibiotics, vancomycin and streptomycin, on newborn mice. They found that streptomycin increased later susceptibility to hypersensitivity pneumonitis – an allergic disease found in people with occupations such as farming, sausage-making, and cleaning hot tubs. Vancoymycin, in contrast, had no effect.
The difference in each antibiotic’s long-term effects can be attributed to how they changed the bacterial ecosystem in the gut.
“This is the first step to understanding which bacteria are absolutely necessary to develop a healthy immune system later in life,” says Dr. McNagny, a member of UBC’s Biomedical Research Centre.
Infants should be treated with antibiotics when needed, Dr. McNagny says, but he hopes these results will help pinpoint which bacteria make us less susceptible to disease. This could open up the possibility of using probiotics to boost helpful bacteria.
“Probiotics could be the next big trend in parenting, because once you know which bacteria prevent disease, you can make sure that children get exposed to those beneficial bacteria,” he says.