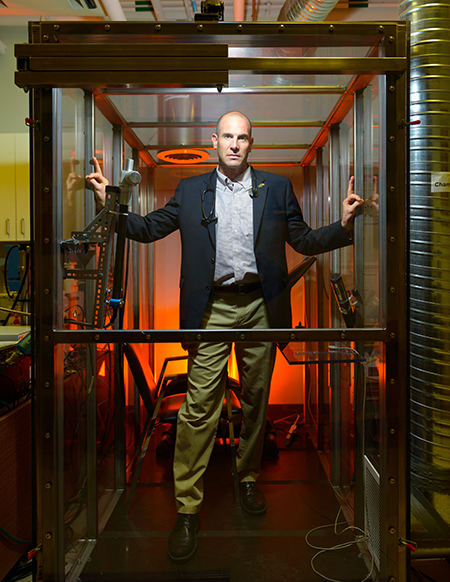
Chris Carlsten in the chamber that simulates levels of diesel exhaust in places like Beijing and busy ports in B.C. Photo: Don Erhardt
Chris Carlsten’s lab is relegated to the basement of a research annex at Vancouver General Hospital, and that’s probably just as well.
First of all, there is the dull rumble of a diesel generator that reverberates throughout the room whenever an experiment is running. Then there is the smell – unnoticed by some, but distinctly detectable by others – of exhaust.
But most of all, there is the polycarbonate-enclosed chamber, about the size of a standard bathroom. In Dr. Carlsten’s experiments, research subjects sit and exercise in the chamber for two hours, inhaling the diluted and aged exhaust that simulates the air quality along highways in such places as Beijing or at busy ports of British Columbia.
This somewhat unnerving set-up, one of only five such pollution labs in the world, is key to Dr. Carlsten’s mission: to establish a definitive link between diesel exhaust and asthma, an intermittent constriction of the lungs that causes chest tightness, shortness of breath, and coughing.
Demonstrating “biological plausibility”
Although there is ample epidemiological evidence that diesel exhaust exacerbates the disease among people who already have it, Dr. Carlsten is using his lab to understand exactly how that happens. One theory he is testing is that diesel exhaust triggers oxidative stress – a chain reaction of harmful chemical reactions that disrupt the normal functioning of cells, particularly their membranes and DNA.
Demonstrating such a physiological proof of damage, he believes, is the only way to get tougher policies enacted. He refers to it as “biological plausibility.”
“To get regulations passed and tighten standards, we need multiple layers of scientific evidence,” says Dr. Carlsten, an Associate Professor of Medicine and the Astra-Zeneca Chair of Occupational and Environmental Lung Disease in the Division of Respiratory Medicine. “While epidemiological patterns and correlations can be very convincing, opponents can dismiss them, claiming there is ‘unmeasured confounding.’ But if you can show it experimentally, and it matches the epidemiology, you’re creating a stronger case that is harder to deny.”
Building a stronger case for environmental modifications – that is the ultimate goal of researchers exploring the molecular and physiological forces underpinning asthma, which affects 8 per cent of Canada’s population, including 486,000 children. Some, like Dr. Carlsten, aspire to influence public policy.
Frozen data
Denise Daley, on the other hand, envisions changes in individual behaviour.
An Assistant Professor in the Department of Medicine, Dr. Daley is leading a five-year study exploring whether early life exposure to cigarette smoke alters the expression of certain genes, and whether that increases susceptibility to asthma. And her research tools, like Dr. Carlsten’s, are relegated to the basement.

Some of the frozen DNA samples that will be used to find a link between genes, smoking and asthma. Photo: Brian Kladko
Stored in industrial-sized freezers at St. Paul’s Hospital set to -80 C are thousands of frost-covered vials, containing blood and blood components donated by parents and children in British Columbia and Manitoba over a 15-year period. The donors also provided information about their health, and in the case of the parents, their smoking habits.
Dr. Daley and her collaborators will use those samples to look for a type of genetic alteration known as methylation, in which a compound of carbon and hydrogen latches onto a part of the DNA. That bonding can enhance or dampen the expression of individual genes, leading to significant changes in how that cell develops and functions.
The connection between parents’ smoking and children’s asthma is already well established, but much like diesel exhaust, it’s a circumstantial case, based on statistics about patterns of behaviour and illness. So even though smoking is a “risk factor” for asthma, it hasn’t proven to be a cause.
Dr. Daley’s team is pursuing the hypothesis that exposure to smoke causes changes in methylation patterns that, in turn, trigger a cascade of reactions leading to childhood asthma, and possibly allergies as well.
A drug, or a dog
In trying to prove that theory, they will try to identify where in the genome that methylation takes place. Using powerful computers, they will then search for patterns and correlations based on data about the donors – whether the parents smoked, whether the children were exposed to smoke in the womb or in early childhood, and whether the children suffer from asthma or allergies.
“What is that mechanism?” Dr. Daley says. “If we know it, we might be able to intervene, depending on the child’s genetic profile.”
Maybe that intervention would be a drug. More likely, it would be a variety of recommendations for the parent that would counteract or mute the effects of the turned-off gene – such as bringing a dog into the home, or removing a dog from the home, depending on the child’s genotype. Other recommendations could touch on diet or physical activity.
“We may have very targeted environmental solutions that may be different, based on what your genes are,” Dr. Daley says.
Of course, recommendations are only as good as the person who is supposed to follow them. Although warnings about smoking – and especially smoking while pregnant – have been enormously effective, some expectant mothers still do it. But if doctors can point to a child’s genetic profile while conveying the need to take certain steps, Dr. Daley believes the message might carry more weight.
“We’re not far from determining a child’s susceptibility,” she says. “If we can identify what types of gene-environment interactions they are susceptible to, then, working with the parents, we might be able to modify their environment.”
Anti-oxidant experiments
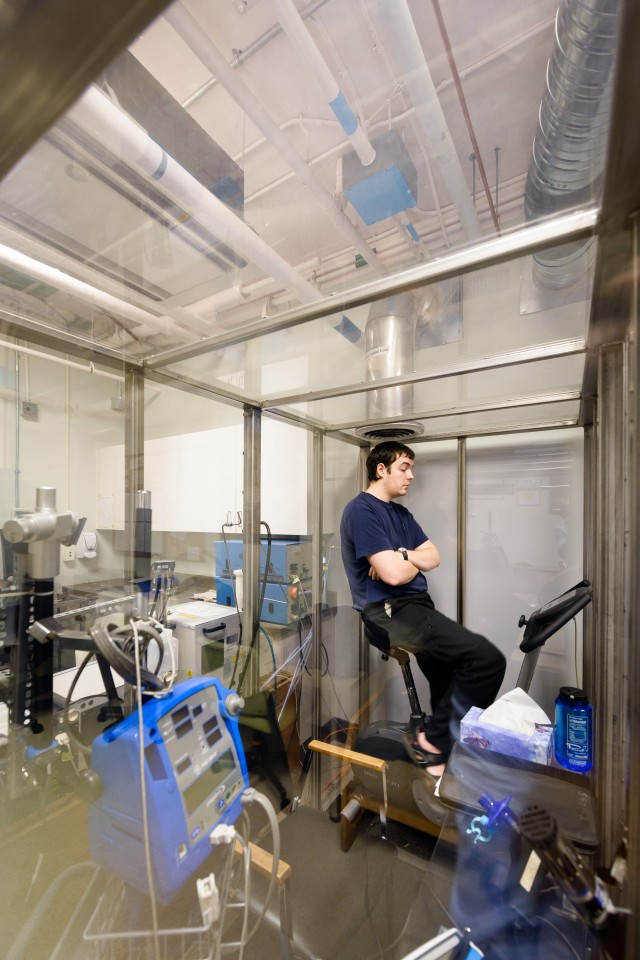
Ryon Anas participates in
an experiment in Chris Carlsten’s Air Pollution Exposure Laboratory. Photo: Don Erhardt
Dr. Carlsten, while believing tobacco use has “no redeeming value” and therefore should be choked off as quickly as possible through bans and taxes, has focused on what might seem a more intractable problem. After all, diesel exhaust isn’t the product of a bad habit, but the product of transportation – the lifeblood of industrialized and developing societies.
All the more reason, he believes, to find the proof of harm. Thus, he maintains a steady stream of volunteers willing to spend a couple of hours – usually several times – in his Air Pollution Exposure Laboratory.
“At the end of the day, any effort to change regulations about diesel exhaust will very likely be challenged in court,” he says. “When you have experimental studies, that changes the whole story very powerfully. If the community believes you’ve demonstrated a mechanism by which harm is inflicted, the effort gains credibility.”
Dr. Carlsten has uncovered solid evidence of his oxidative stress theory, by giving his subjects anti-oxidants before exposing them to exhaust. The result: their lungs don’t constrict as much as they do when not given antioxidants. He also has found that exhaust exposure causes a rise of a type of micro-RNA that plays a role in immunity (and thus inflammation), and that anti-oxidants prevent that increase.
While it’s reasonable to think that anti-oxidants might thus have potential as a preventive therapy for asthma, Dr. Carlsten would rather see the findings used to justify a requirement for diesel engines to produce fewer oxidizing particulates.
“I’m not a big supporter of anything that seems like a treatment, because that’s avoiding the fundamental problem,” he says. “It’s much more important to me to validate the plausibility of what we’re seeing epidemiologically, so we can decrease air pollution and protect the entire population.”
