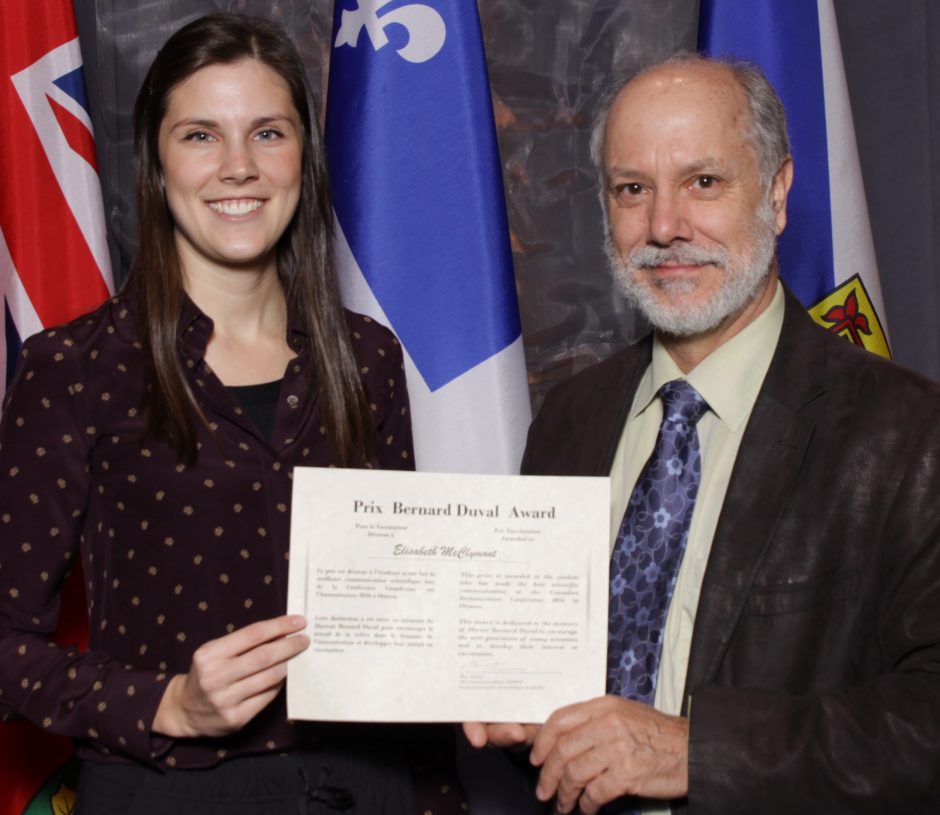
Elisabeth McClymont receiving the Bernard Duval Award from Shelley Deeks, Medical Director, Public Health Ontario & Chair, Vaccinology Student Research Program.
Elisabeth McClymont, a graduate student in the UBC Department of Obstetrics and Gynaecology, won the top student prize at last month’s Canadian Immunization Conference for her research on the efficacy of the human papillomavirus (HPV) vaccine in women who are HIV-positive.
McClymont explored the vaccine’s efficacy because women who are HIV-positive experience higher rates of HPV infection and cervical cancer than women who are HIV-negative. In addition, people who are HIV-positive have shown to have weaker immune responses to other vaccines.
Seventeen students across Canada submitted applications to the Vaccinology Student Research Program, and 11 students were awarded a travel bursary to attend the conference in Ottawa. Projects were evaluated based on pertinence to immunization programs in Canada, the methods used as well as originality, timeliness and effort involved.
McClymont and the others presented their data in an oral poster session and discussed their research with experienced Canadian vaccinology researchers. McClymont was the sole student selected as the recipient of an educational bursary from the Dr. Bernard Duval Foundation.
“I didn’t have the pleasure of meeting Dr. Duval myself, but I hope to emulate his rigorous approach to science, and to inspire, collaborate and share kindness the way that he did,” McClymont told the 900-member audience at the conference Dec. 8.
McClymont, who is supervised by Executive Vice Dean Deborah Money, tracked the health of more than 400 girls and women who were HIV-positive and received three doses of the vaccine from 14 sites across Canada. The median follow-up time was two years.
Her results are promising: Although the rate of persistent quadrivalent HPV was 2.13 times higher than the previously-reported rate of an HIV-negative cohort, that difference was very low and not statistically significant.
“We’ve seen good short-term efficacy,” she told the gathering. She also noted that there have been no cases in the HIV-positive cohort so far of high-grade squamous intraepithelial lesions, which are risk indicators of squamous cervical cancer.
The study, funded by the Canadian Institutes of Health Research and the Canadian HIV Trials Network, is ongoing.
McClymont’s work is a part of the ground-breaking work by members of the Faculty of Medicine who are part of a BC HPV Research group, a world-leading research collaborative that aims to eradicate cervical cancer.
“I am very proud of the work that McClymont and our team has produced, which is going to lead to our understanding of how to prevent cervical cancer in the most vulnerable populations of women globally, those living with HIV who may not always be able to access preventative screening programs,” Dr. Money said.
Two years ago, UBC researchers and members of the BC HPV research group produced data that was the basis for decisions by the World Health Organization and the European Commission to endorse a schedule of two doses of the HPV vaccine to girls – once between the ages of 9 and 13, and then six months later. That move, from a recommendation of three doses, is likely to make the vaccine more affordable to low-income countries and increase usage in industrialized nations.